Abstract
Introduction
The recent approval of direct oral anticoagulants (apixaban, dabigatran and rivaroxaban) for the risk reduction of stroke for nonvalvular atrial fibrillation, venous thromboembolism (VTE) prophylaxis and treatment opened up more choices of oral anticoagulants for the clinician to choose from, in addition to warfarin. This presents a unique opportunity to study practice trends and to examine preferred use, bleeding complications and length of stay (LOS) at a teaching hospital.
Methods
This was a retrospective single center analysis of the prescribing pattern of oral anticoagulation at Winthrop University Hospital from January 1, 2016 to June 30, 2016. Patients were identified by CareFusion Medmined Surveillance software. Inclusion criteria were > 18 years and initiated on apixaban, dabigatran, rivaroxaban, or warfarin. Exclusion criteria included oral anticoagulant change or discontinuation during hospitalization, pregnancy, and patients who were transitioned to hospice or expired during their hospital stay.
The primary endpoint was to evaluate the patterns of use for oral anticoagulation. Secondary endpoints included determining the indication for anticoagulation, LOS from initiation of anticoagulation, and major bleeding events. Major bleeding events were defined by a drop in hemoglobin >2 grams/dL, or overt signs of a gastrointestinal bleed.
Results
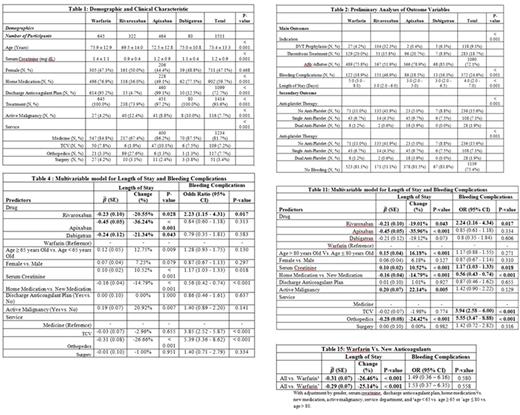
A total of 1511 patients (apixaban 464, dabigatran 80, rivaroxaban 322 and warfarin 645) were included in this study. Patients treated with warfarin had significantly higher serum creatinine compared to all other groups. Patients treated with rivaroxaban had significantly lower serum creatinine compared to patients treated with apixaban (Table 1).
There was an increasing trend towards initiating apixaban for thrombosis treatment and atrial fibrillation/flutter compared to DVT prophylaxis with warfarin (Table 3). Patients treated with rivaroxaban were more likely to have bleeding complications (151 patients, 46.9%) compared to apixaban (86, 18.5%), dabigatran (13, 16.3%) and warfarin (122, 18.9%) with p value <0.001. Patients treated with warfarin had a significantly longer LOS (5 days, 3- 8), compared to apixaban (3 days, 2 - 5), dabigatran (3 days, 2 - 6.5) and rivaroxaban (3 days, 2 - 6), p value < 0.001 (Table 2). Rivaroxaban showed decreased LOS by 20.6%, apixaban by 36.2% and dabigatran by 21.3% when compared to warfarin (Table 4). Patients >80 years had 16.18% increase in LOS compared to patients < 80 (Table 11). Post hoc analysis revealed that there were no differences in the odds of bleeding complications in the new anticoagulants compared to warfarin in the multivariable model after adjustment. (Table 15)
Conclusions
Despite the availability of direct oral anticoagulants, warfarin is still widely used in the hospital setting (43%). This is especially true in patients with renal insufficiency where the use of rivaroxaban and dabigatran use is contraindicated. The most common indication for oral anticoagulation at our center was for atrial fibrillation. Rivaroxaban was associated with the highest incidence of bleeding. Treatment with apixaban, dabigatran and rivaroxaban demonstrated a significantly decreased length of stay compared to warfarin and may result in significant cost savings for the hospital.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal